Very fundamental, indeed
💬 comments
We're going to need some IV hydralazine after reading this.
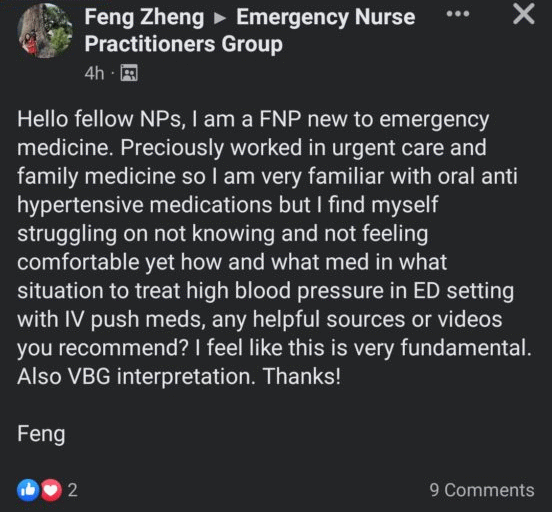
As a recent public opinion survey co-sponsored by the American College of Emergency Physicians (ACEP) found, the vast majority of adults prefer physician-led care in an emergency, with only 9 percent (inexplicably) stating that they preferred a nurse practitioner. If this post by midlevel family nurse practitioner Feng Zheng is any indication, it's certainly not hard to see why physicians lead.
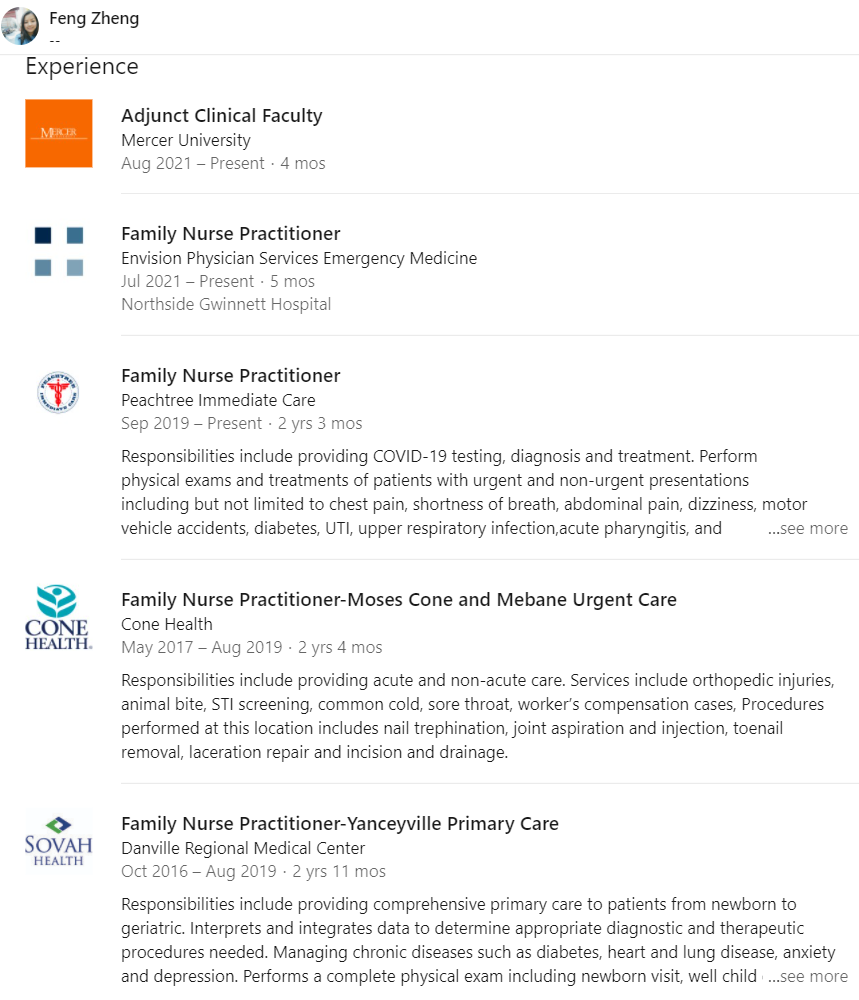
One might wonder why in the holy hell a family NP is working in an emergency department, let alone a Level II trauma-certified ED in a fairly sizable, 353-bed hospital such as Northside Hospital Gwinnett. In a perfect and ideal world, emergency departments in the United States would be exclusively staffed by physicians. But in the modern reality of healthcare capitalism, for-profit hospitals, and staffing groups completely infiltrated by private equity (including Envision, of course), one would be hard-pressed to find an ED in the US without some form of midlevel coverage. Unfortunately, this is especially true for EDs located in more rural or less-desirable areas. A common (perhaps the most common) arrangement is for ED midlevel NPs and PAs to staff so-called "fast-track" areas limited to patients with benign or low-acuity complaints that would otherwise be appropriate for urgent care.
Needless to say, a patient who requires IV antihypertensives or a VBG does not fall into the "fast-track" category and should be exclusively seen and managed by an ED physician. And as any emergency medicine physician practicing within the past decade would know, in the absence of any other indications (e.g. hypertensive emergency), there is little evidence to support immediate intervention in the ED for asymptomatic high blood pressure. In fact, there's an ACEP Clinical Policy regarding this very topic:
Patients referred to the ED with asymptomatic hypertension DO NOT need immediate blood pressure management or lab screening, but do need referral to a primary care physician for repeat blood pressure checks and initiation of pharmacologic therapy if needed.
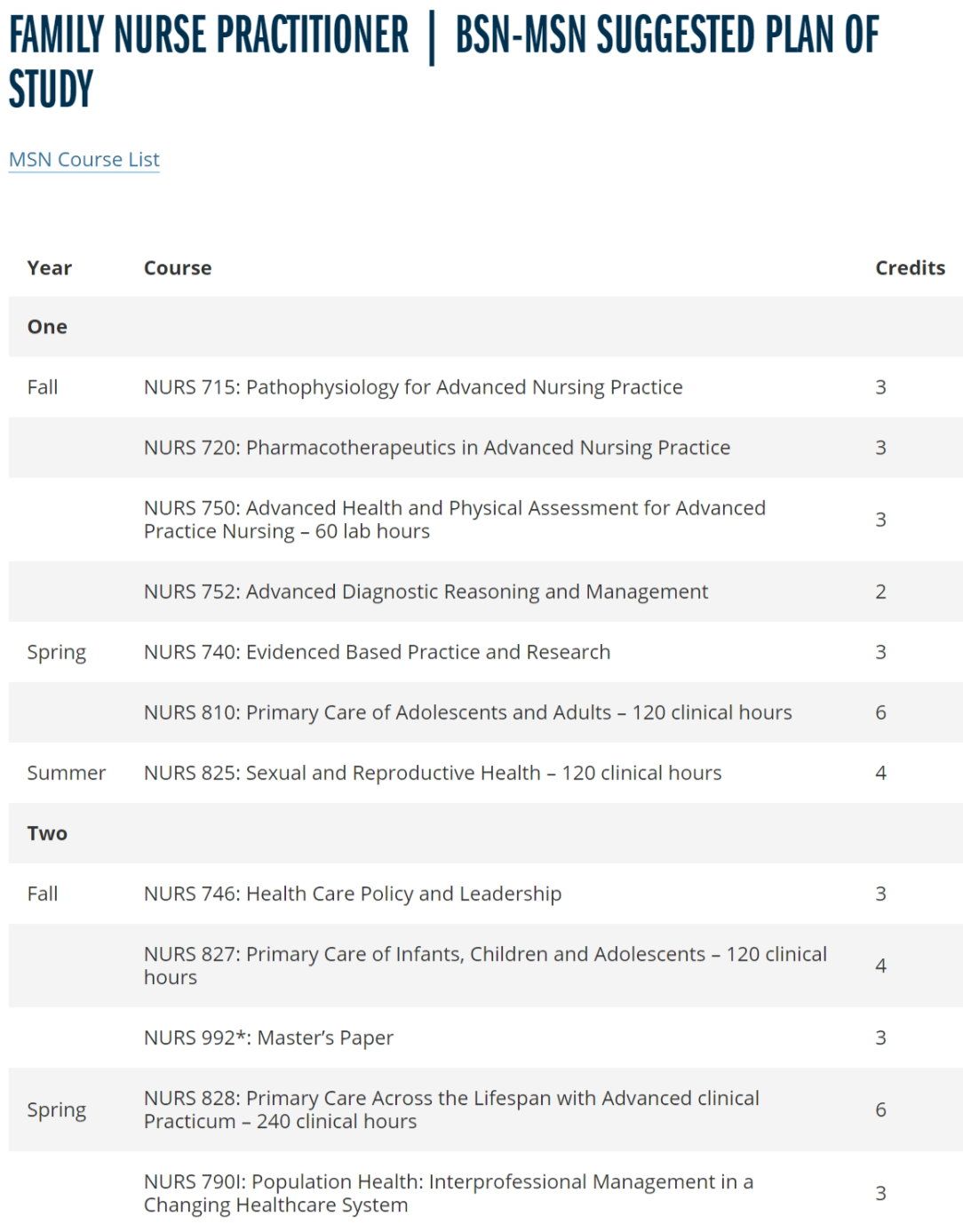
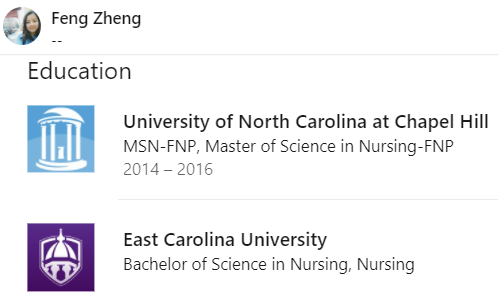
Then again, who's got time to learn basic emergency medicine and peruse clinical guidelines when you only have ~600 clinical hours of training, with the rest of your curriculum composed of bullshit classes on "Health Care Policy and Leadership" and writing useless "Master's Papers"? Not that anything EM-related would be covered in a FNP program, anyway. There's a reason why emergency medicine and other fields such as family medicine and internal medicine are considered distinctly different medical specialties, with discretely separate residency training pathways for physicians. There's a reason why physicians can't just decide to practice primary care one day and become a surgeon tomorrow, unlike how midlevel NPs and PAs can seemingly cut-and-run to a new specialty faster than the US military out of Afghanistan. There's a reason why medical school curricula are substantially longer and vastly more intense than that of NP school. Turns out, you need a lot more than online school and a few hundred hours of clinical exposure to practice medicine competently.
Oh, what's that? Is that the sound of former AANP president Sophia Thomas, DNP, APRN, FNP, PPCNP, FAANP nebulously claiming with a straight face that nurse practitioners practice not medicine, but healthcare?