Insubordinate NP student goes behind cardiologist's back, sends patient to ER instead of home
💬 comments
We apologize in advance if you go into supraventricular tachycardia while reading this article.

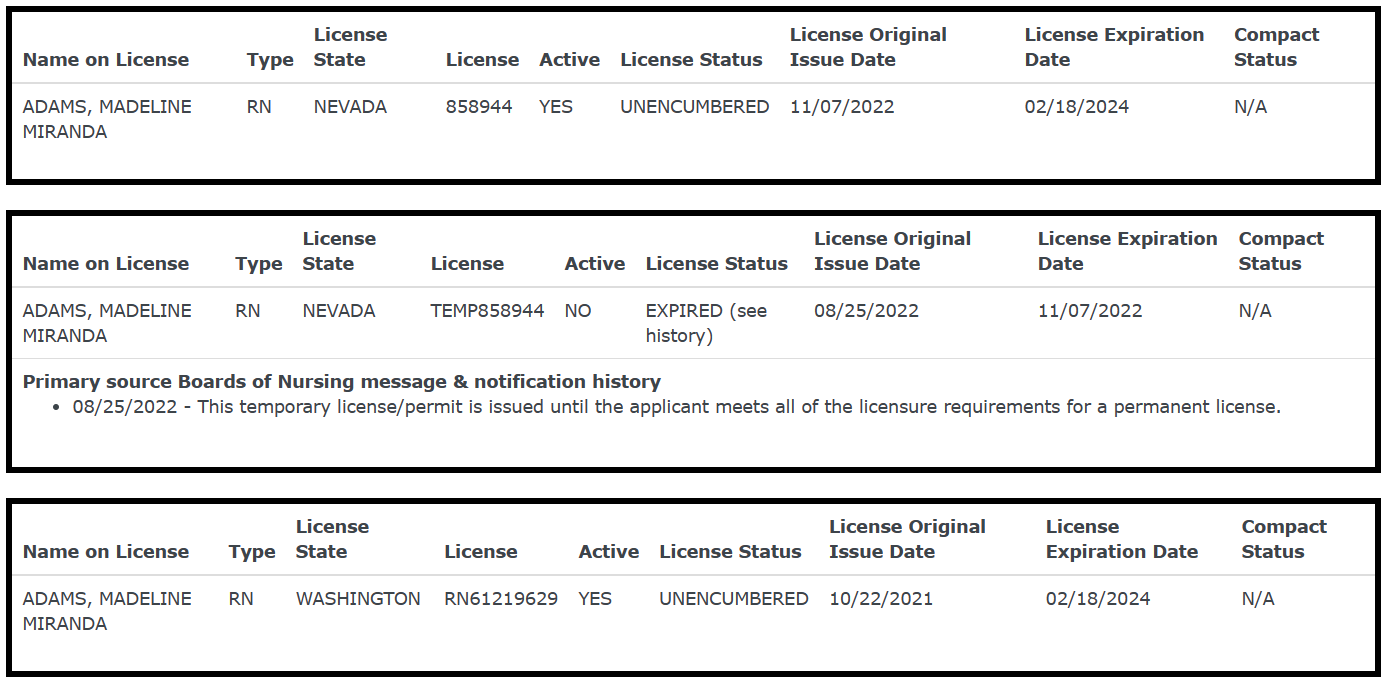
Here at Midlevel.WTF, we're all well aware of the risks posed by incompetent and uneducated midlevels practicing without supervision. But just as dangerous are midlevels who actively undermine the patient care plans and directives of their supervising physicians. While direct patient harm is certainly the primary concern, no physician wants their medical license jeopardized because one of the midlevels under their command decided to go off the reservation. Today, we bring you no finer example of this than this incident involving midlevel nurse practitioner (student) Maddie Bristol a.k.a. Madeline Miranda Adams, who made the brilliant decision to self-document her act of flagrant insubordination on Facebook.
Just imagine what would happen if a medical student or resident decided to pull a stunt like this and deliberately disobey a direct order from their attending physician. At a minimum, the trainee would get a very stern reprimand or maybe even fail the rotation. If the insubordination resulted in egregious patient harm, the trainee would likely be dismissed from medical school or terminated from residency.
Notwithstanding the fact that going completely behind your supervising physician's back (there's no "kinda" here) is just totally fucked up, Ms. Maddie's medical decision-making is just plain wrong, even from the few nuggets of information we can glean from her post. But then again, wouldn't it be presumptuous to think that a FNP/PMHNP, let alone a student NP, could come remotely close to holding a candle to a seasoned cardiologist who has completed, at the very minimum, four years of medical school, three years of internal medicine residency, and three years of fellowship training in cardiology? And yet, here we are.
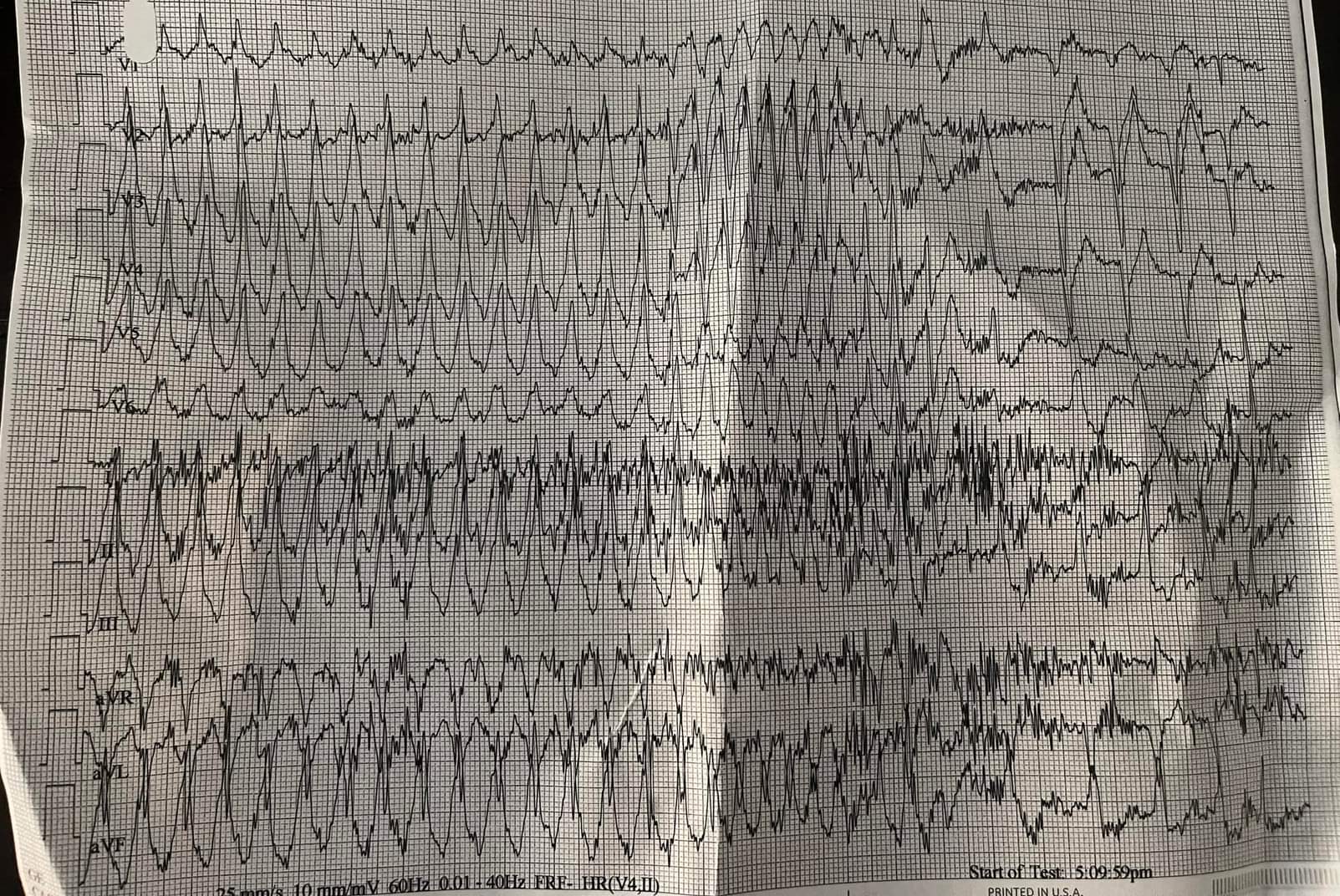
Most tellingly, it is plainly obvious that Ms. Maddie has little, if any understanding of basic cardiology and arrhythmias even when the textbook-appearing 12-lead EKG is staring her in the face. In her own words, the patient "kept going in and out", "the longest run was 24 beats", and "as time went on the runs got shorter". Golly, if only there was a specific medical term for that sort of arrythmia that even a fourth-year medical student would know...

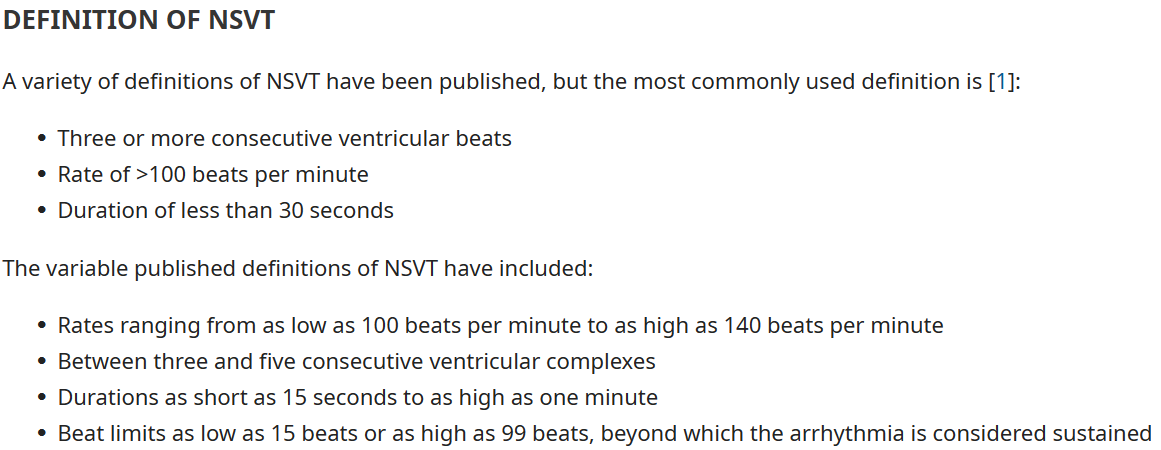
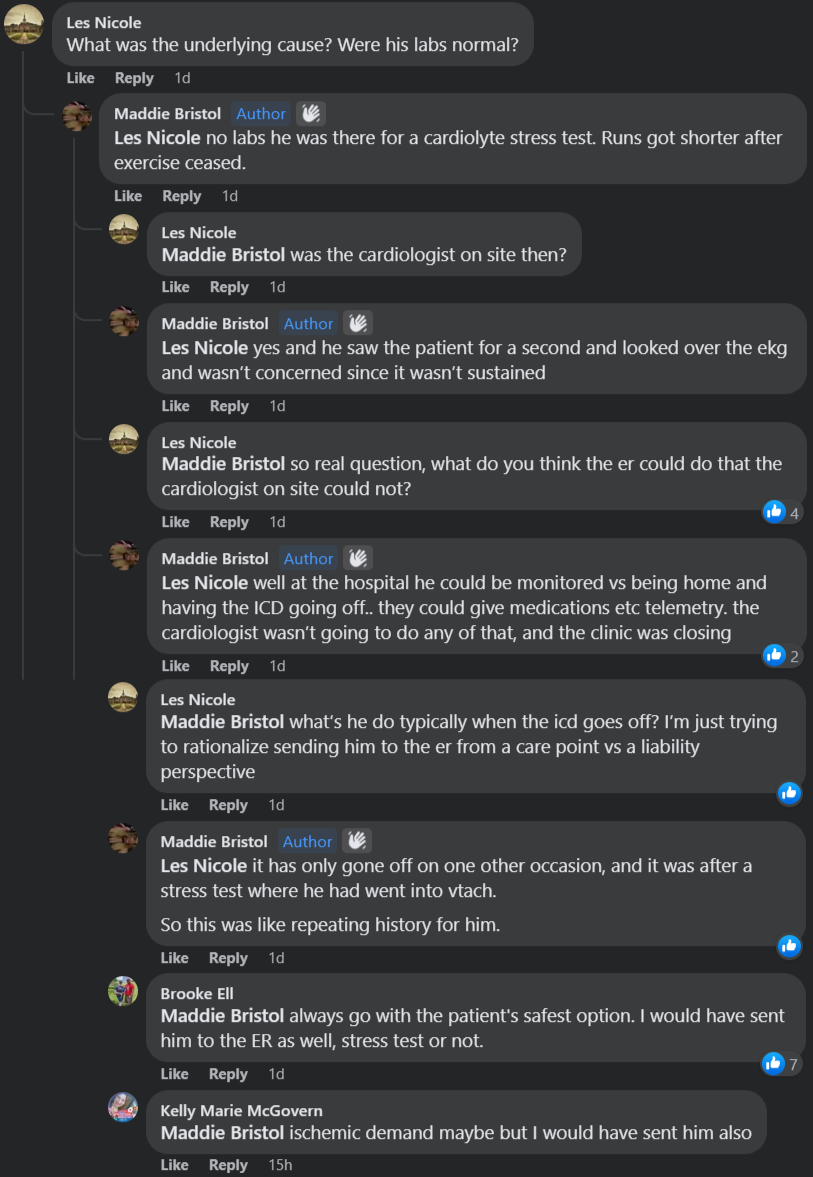

From the follow-up Facebook comments, which are in and of themselves mind-numbingly painful to read, it turns out that the patient's asymptomatic NSVT was inducible following a chemical stress test. Needless to say, this is much less concerning, especially if it's happened only once before under similar circumstances. Unlike this smooth-brained student NP, we are more than willing to bet that these are all factors the cardiologist silently considered using his numerous gyri and sulci before deciding to send the patient home. Seriously, Ms. Maddie, why the flying fuck do you think this patient who, again in your own words, "has an EXTENSIVE history including prior cardiac arrests associated with vtach" even has an AICD in the first place? Maybe she thinks that a few rounds of ACLS including chest compressions, manual defibrillation at 200 J, and epinephrine are a better alternative?
In any case, let's humor Ms. Maddie's brilliant idea to disobey her supervising cardiologist and send this asymptomatic NSVT patient to the ED. What the hell does she think the emergency physician (at least, we hope it's a physician and not another midlevel) is going to do? Hmmm...maybe consult the patient's cardiologist (who, by now, is probably going to realize he just got backstabbed by his own NP) and eventually send the patient home as originally intended? And if the ED can't get in contact with the patient's own cardiologist and ends up speaking with someone on call who's unfamiliar with the patient, there's a decent chance this patient might end up getting admitted for a completely unnecessary observation stay, replete with all of the unpleasantries and risks of hospitalization.

Either way, the patient is going to end up on the hook for all of the expenses associated with the ER visit and/or hospital stay. No wonder hospital administrators love employing armies of midlevels - as we see here firsthand, medical incompetence and insubordination is great for the bottom line. It's value-based care at its finest!
So to answer your question, Ms. Madeline, no - you did NOT do the right thing. You did the completely wrong thing!


