ER NP places a STAT Facebook consult for compartment syndrome
💬 comments
Clearly, asking the Facebook peanut gallery for help during a limb-threatening surgical emergency is the most appropriate course of action.

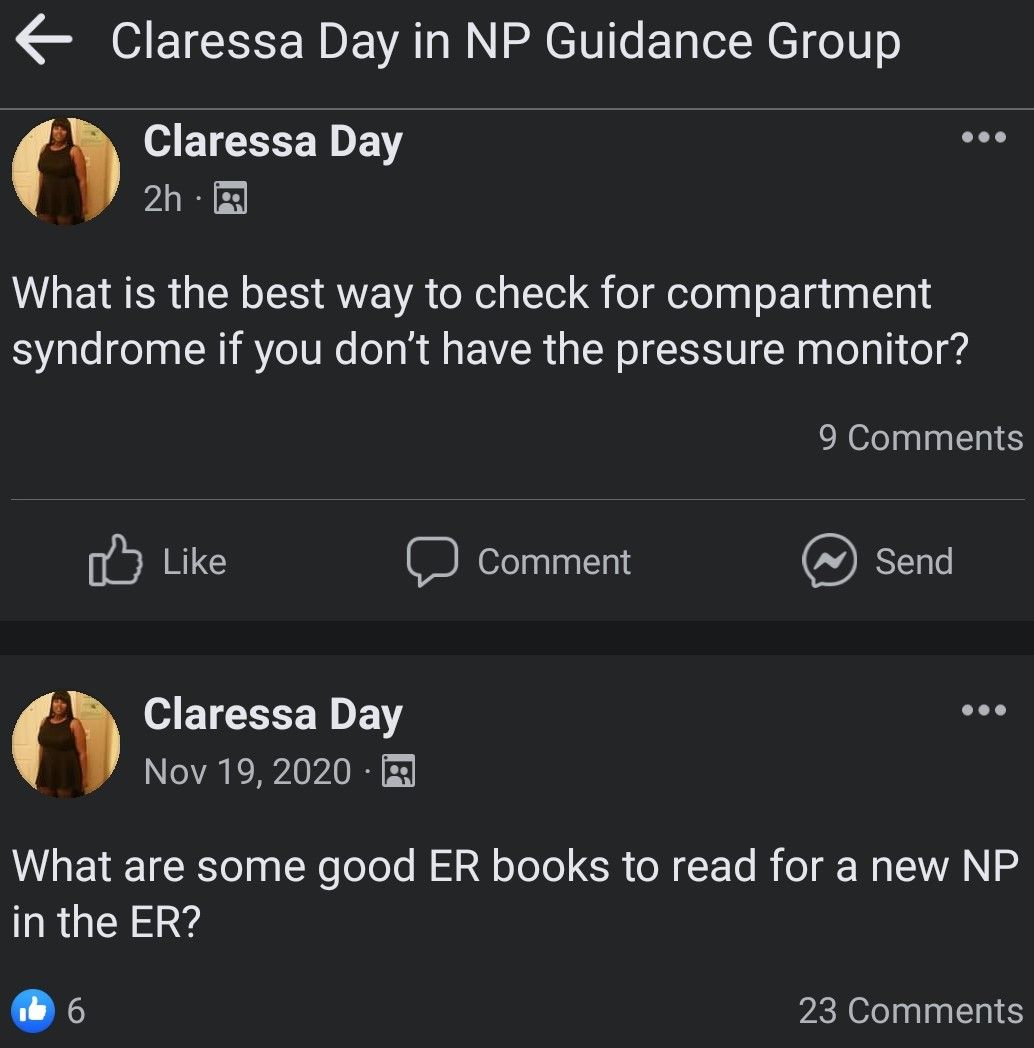
It goes without saying that an emergency medicine physician should be able to instantly recognize emergent, life- or limb-threatening conditions. Unfortunately, as the post above from FNP Claressa Day (Hawkins) demonstrates, one can't trust that midlevels working in the ED are capable of doing the same. FNP Claressa, who appears to work at the storied John H. Stroger Jr. Hospital of Cook County in Chicago, is a bit confuzzled when it comes to compartment syndrome.
For our layperson audience, acute compartment syndrome is a limb-threatening surgical emergency that develops when the internal pressures within a muscle group builds to dangerous levels (e.g. due to swelling or bleeding), compromising blood flow to the surrounding muscle tissue and nerves. It's classically associated with fractures or crush injuries, particularly in the leg. The standard treatment is an emergent surgical fasciotomy.

Any second-year medical student who paid attention in class would be able to recite the six P's of compartment syndrome: pain, pallor, pulselessness, parasthesias, paralysis, and poikilothermia, of which more concerning symptoms such as pulselessness and paralysis are late findings indicative of irreversible damage to muscle and nerve tissue. Indeed, the diagnosis of compartment syndrome has historically been overwhelmingly clinical. Thanks to the wonders of modern medicine, tools like the Stryker Intra-Compartmental Pressure Monitor System allow for the direct measurement of compartment pressures to confirm a diagnosis of compartment syndrome. However, while compartment pressure measurement is a useful confirmatory adjunct, there is no damn way in orthopedic hell that it should be used as a first-line tool to diagnose compartment syndrome. Anyone who can't diagnose a clinically obvious compartment syndrome without using a pressure monitor has no fucking business working anywhere near an emergency department. Just imagine if a trauma surgeon asked for a CT scan to confirm a blatantly obvious gunshot wound. Pathetic!
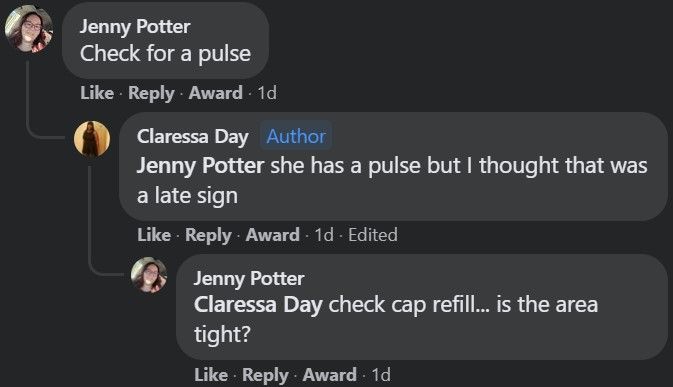
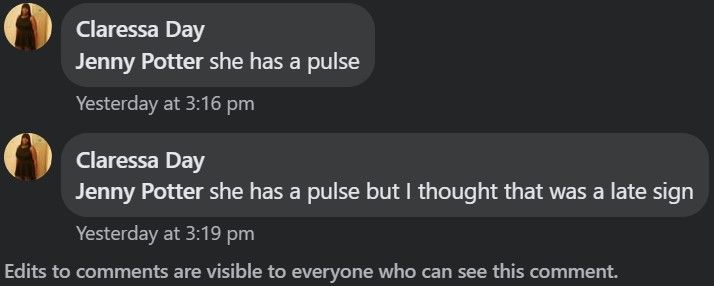
As previously stated, acute compartment syndrome is a surgical emergency, and every minute counts. If unrecognized and left untreated, it may ultimately result in the need for limb amputation. If the diagnosis is suspected, you should be on the phone putting out a STAT page to the surgery team, not diddling around asking for help on Facebook. With this in mind, it's worth taking a close look at the timing of the post - the original post was made on 12/24/2021 at 3:09 PM EST, and FNP Claressa's initial response to the comment about checking for a pulse was made only seven minutes later at 3:16 PM. Did she run back to the patient's exam room after seeing NP Jenny Potter's comment, check for a pulse, and then post the findings on Facebook? What would she have done if the patient's extremity didn't have a pulse? Wait for the next random person to reply on Facebook instead of paging the surgery team? God only knows.

Needless to say, social media consults like this reflect badly not only on the midlevel in question, but on the entire midlevel nurse practitioner profession as a whole. Why don't these midlevels ask their physician superiors? Obviously, this doesn't apply to rogue midlevels running amok and practicing independently in areas with full practice authority, but certainly, at a Level I trauma center such as the guns-and-knives club that is Cook County, there should be no shortage of distinguished and seasoned emergency medicine physicians to ask for help. Indeed, as any EM physician would know, Cook County is home to one of the nation's premier emergency medicine residency training programs. Surely, none of their 80 highly accomplished resident physicians would be caught dead asking a question like "the best way to check for compartment syndrome if you don't have the pressure monitor". The midlevels at Cook County are clearly not cut from the same intellectual crust as the physicians. Coincidentally, "checking for a pulse" seems to be the standard these days for getting into NP school. Are midlevels scared that their educational inadequacy and clinical incompetence will be exposed if they ask their help? In any case, in the end it's the patient that suffers.
