ER NP checks labs, finds "no acute abnormality"
💬 comments
It's not like hypokalemia can be dangerous or anything.
It's not every day that we get an opportunity to live up to our motto and directly examine a chart signed by a midlevel. Expounding upon our previous post "Independent, unsupervised NPs don't belong in the emergency department", today's case comes courtesy of a little birdie with substantially more knowledge, training, and experience than the midlevel family nurse practitioner featured below.
First, some backstory: we have an elderly patient who was sent to the emergency department due to vomiting and an ability to tolerate oral intake. We've since been informed that the patient in question had also been hospitalized recently in the past few weeks for severe hypokalemia (K = 2.1).
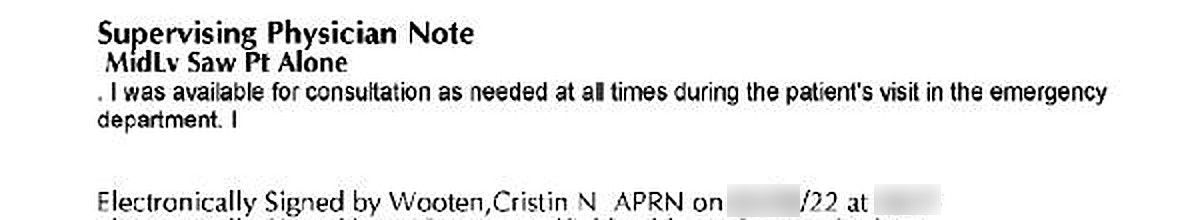
From the patient's ED visit, we have the labs, free-text re-evaluation and medical decision-making (MDM) notes, and a signed attestation clearly stating that the patient was seen alone in the ED by a midlevel provider, FNP Cristin Wooten.
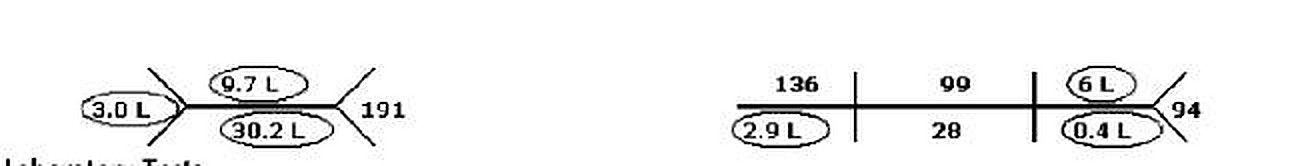
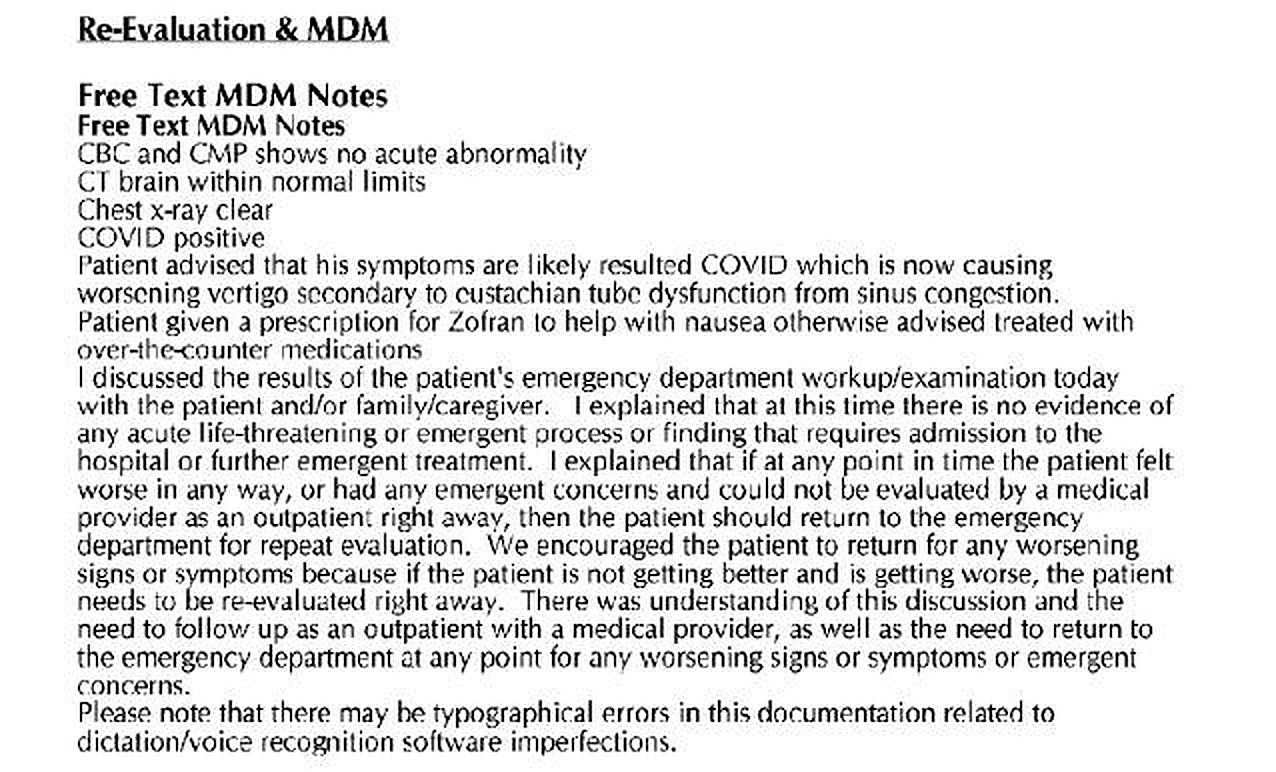
Wow - besides the sophomoric gender mismatch, there are so many questionable things to unpack here. First off, it's hard to believe the statement that "CBC and CMP show no acute abnormality" when more than half of the lab results are circled because they are abnormal. With a hemoglobin of only 9.7, this patient is obviously anemic. This could certainly be chronic, although there's no documentation to suggest any review of previous values. But there is no way in hell that one could write off a potassium level of 2.9 mEq/L. Yet, there's nothing at all in the midlevel's MDM acknowledging this electrolyte abnormality, the patient's history of hypokalemia, any administration of supplemental potassium, or any mention of additional workup such as obtaining an EKG or checking a magnesium level. Especially in a patient with severe nausea/vomiting, this is particularly concerning, given that this patient's levels are not far off from where potentially fatal cardiac arrythmias might start to manifest. In a patient unable to tolerate oral intake due to nausea/vomiting, IV potassium replacement would be indicated. For fuck's sake - recognizing and replacing abnormal electrolytes is medicine 101!
Furthermore, there's no mention at all of any differential diagnoses in this 75-year-old patient with nausea/vomiting. Even in the absence of chest pain or shortness of breath, a first-year emergency medicine resident on day 1 of residency would at least consider the possibility of acute coronary syndrome and entertain ordering an EKG and troponin in an old lady who's vomiting to the point of not being able to hold anything down. Speaking of which, we don't see any documentation at all regarding specific management or resolution of the patient's nausea/vomiting. Did the patient get any IV fluids? Was a P.O. challenge performed to ensure that the patient could tolerate oral intake before being sent home with instructions to just Zofran and chill? As the old medicolegal adage goes, if it wasn't documented, then it didn't happen! And why bother obtaining a CT head if you're just going to attribute the patient's symptoms to "worsening vertigo"? Did the patient have an abnormal neurological exam to warrant head imaging? Was a HINTS exam performed to elicit for central causes of vertigo? Was there concern about a stroke or intracranial pathology? And seriously - "eustachian tube dysfunction from sinus congestion"? Well hot diggety damn, didn't that meandering diagnosis come out of left field! Did this midlevel NP consider that this apparently COVID-positive patient's GI symptoms might merely be due to fucking COVID itself? Jesus fucking overcomplicated Christ. And even if this was peripheral vertigo, why the fuck wasn't the patient symptomatically treated for that with Antivert?
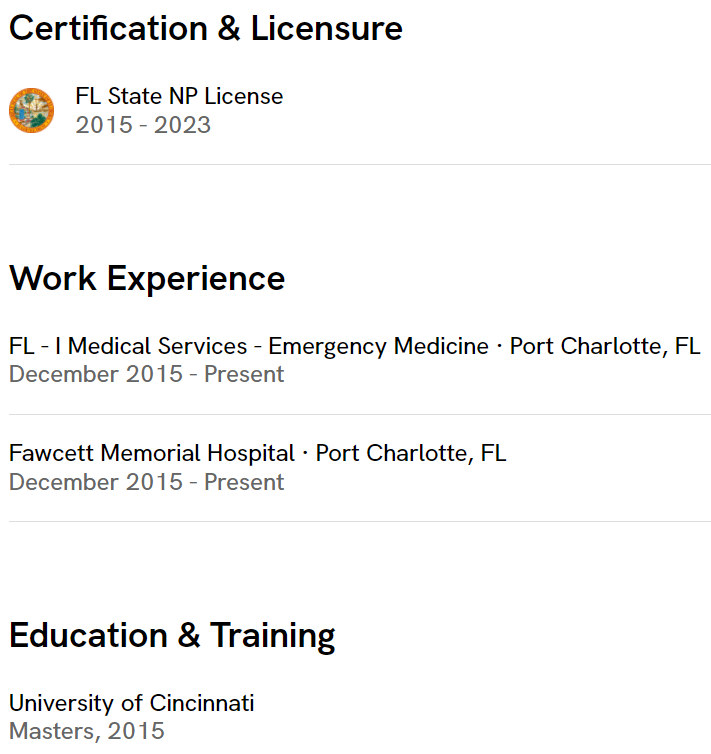
Some online research and a query of Florida's nursing board reveal that the midlevel in question, Cristin Wooten, appears to be employed at Fawcett Memorial Hospital in Port Charlotte, Florida. This 238-bed, for-profit acute care hospital is owned by the McDonald's of healthcare, Hospital Corporation of America (HCA). Its emergency department appears to be staffed under a contract held by Envision, the corresponding McDonald's of physician (and midlevel) staffing.
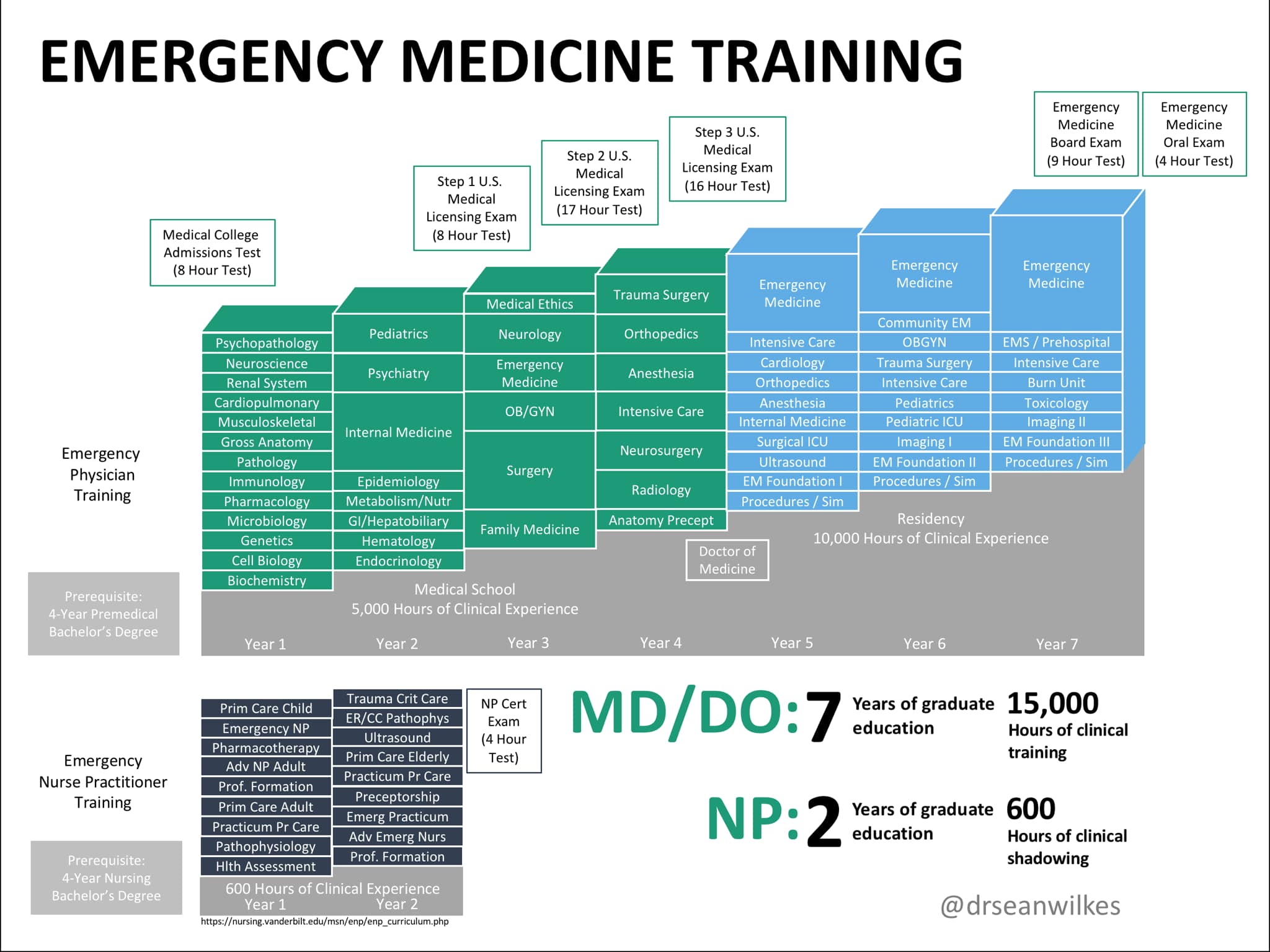
We hate to keep beating a dead horse, but once again, one can conclude that a midlevel nurse practitioner is no substitute for a physician, certainly not in the emergency department where potentially life-threatening pathology can lurk around every corner. The American Association of Nurse Practitioners and other midlevel lobbies love to furiously masturbate to the (false) idea that midlevels are capable of providing care that is equal to or better than that provided by physicians and should therefore be allowed to practice independently. However, as the above example shows, this is simply not the case. At least on paper, a supervising physician was present, but he/she never saw the patient, and there's no documentation whatsoever that the supervising physician was ever made aware in real time of the patient's lab results. And therein lies the problem: in what universe would a physician consider a potassium level of 2.9, in a patient with intractable vomiting no less, to not be an acute abnormality? Unfortunately for patients, this is the shit-tier standard of care one can now expect these days from a midlevel provider in the emergency department where your life could potentially be on the line.
