A "real" PMHNP worries about the fake ones
💬 comments
The "real" PMHNPs? How about the real psychiatrists?

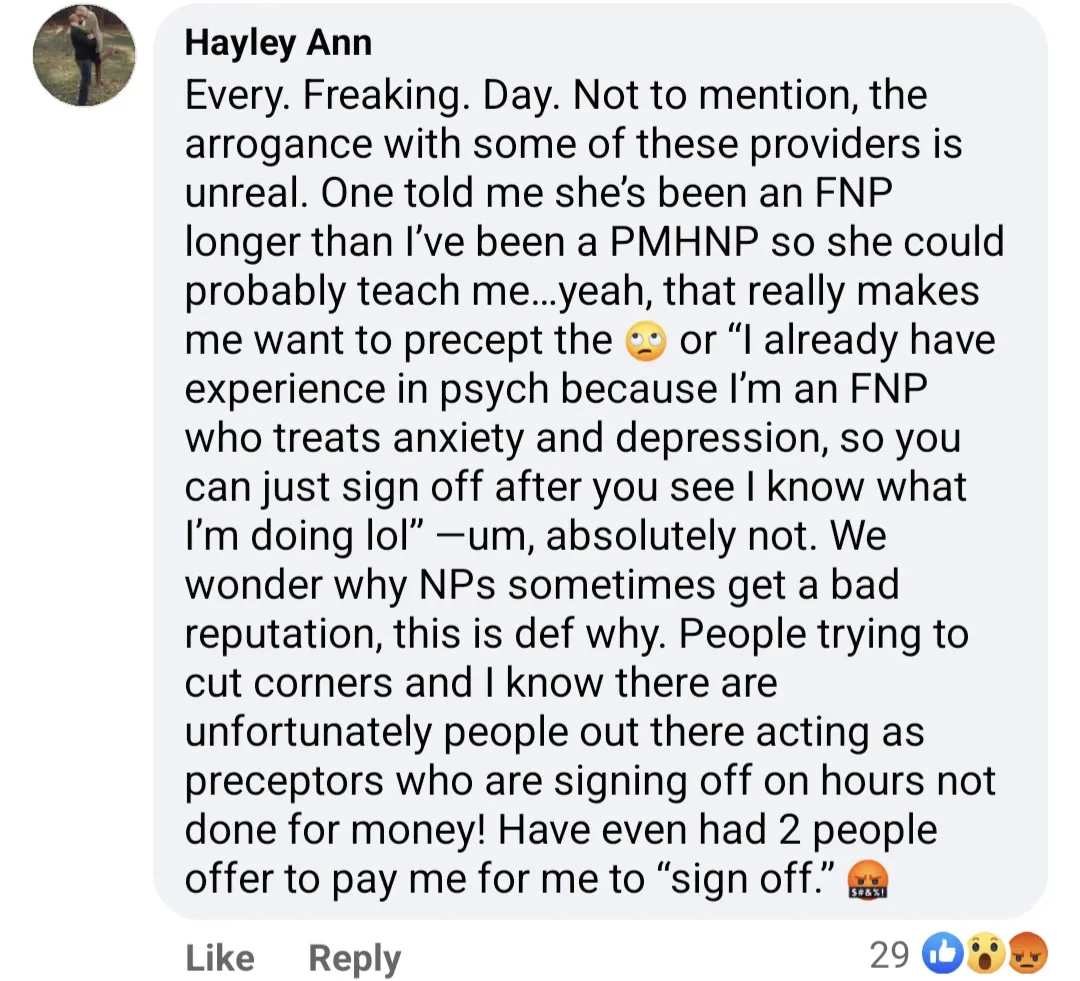
It's always fuckin' hilarious when a nurse practitioner starts bitching about the quality of the education received by others in their profession. "Pot calling the kettle black"? "People in glass houses shouldn't throw stones"? Whatever snarky idiom you wish to "emerse" yourself in, physicians have been ringing the alarm bells for years when it comes to the shit-tier education provided by nurse practitioner programs as well as the nonexistent admissions standards that accompany many of them. Meanwhile, actual interest or passion in the field is an afterthought. Especially with diploma mills such as Walden University, Chamberlain University, and similar "universities" of their ilk, the financial motivations of both the student and the institution are front and center - the student is looking to fork over some tuition money in exchange for an easy, guaranteed clinical degree that potentially unlocks the door to a six-figure salary, while the diploma mill is looking to make a quick buck by selling said degree and minimizing "unnecessary" expenses. Why bother with the unnecessary expense of securing high-quality clinical rotations when you can pass the cost of doing that to your own student-customers? They can just bribe pay a NP friend preceptor in exchange for a passing grade! It's all about pencil whipping, er, box checking!
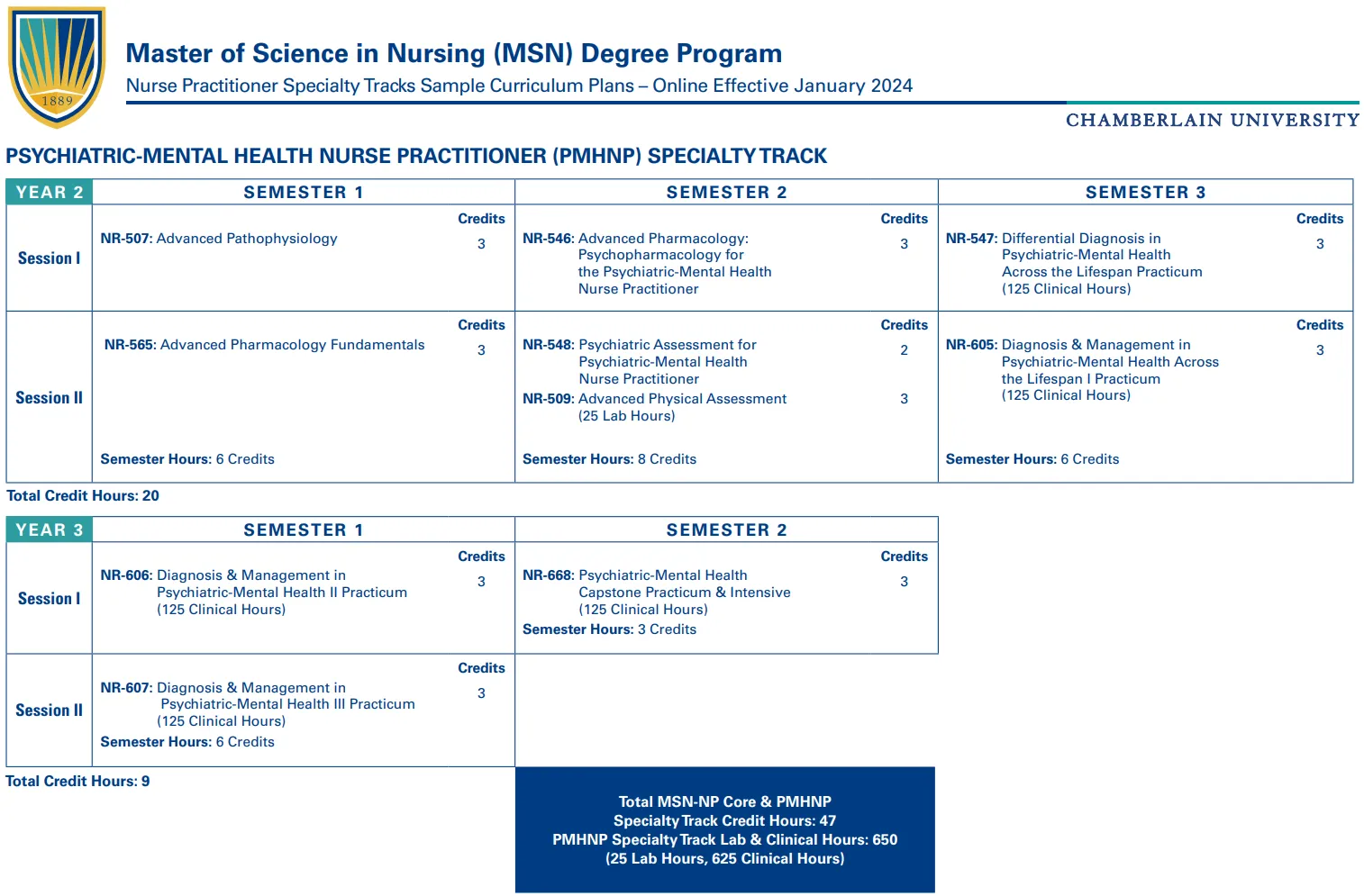
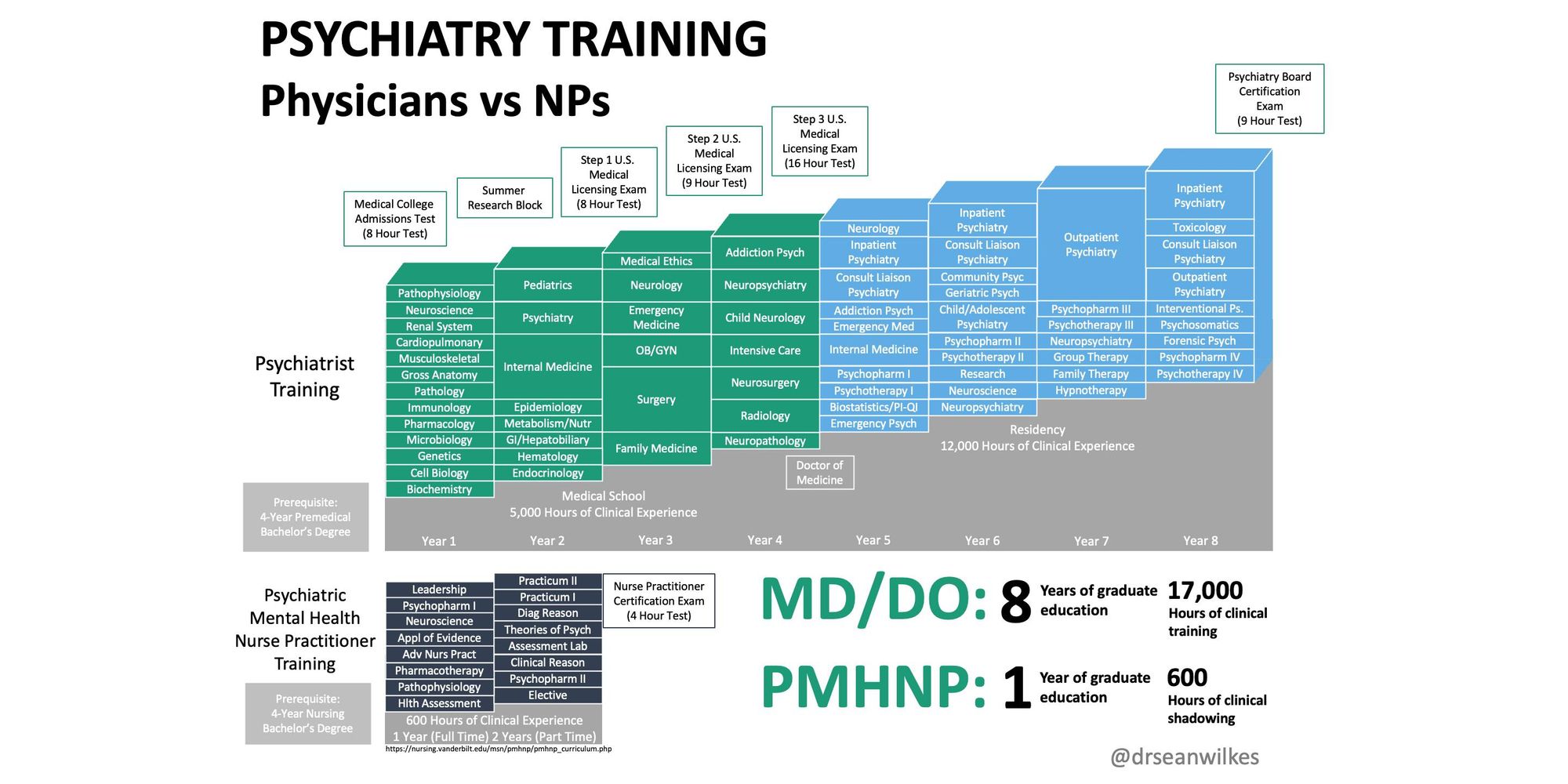
Indeed, with the typical psychiatric-mental health nurse practitioner (PMHNP) program only requiring a couple years of 100% online education and 600-700 clinical hours, the educational rigor of such programs is literally a complete fucking joke when directly compared to the educational journey of a board-eligible/board-certified psychiatrist, as evidenced by the eye-opening diagram above created by fellowship-trained psychiatrist Sean Wilkes, MD. Based on clinical training hours alone, the average newly-minted PMHNP these days has ~3.5% of the knowledge, training, and experience of a psychiatrist.
But what we really need to discuss here is the rampant rise of so-called post-master's certificate programs that essentially allow nurse practitioners to change specialties at the drop of a fucking hat. Tired of working in primary care as a family nurse practitioner (FNP)? Looking to become a PMHNP because you think psychiatry is "easy" and you're aspiring to make bank by opening your own online ADHD pill mill in a full practice authority state without having to be supervised by an annoying physician? Just do a psychiatric-mental health NP certificate program! These certificate programs are offered by all of your favorite diploma mills, and perhaps not surprisingly, even being pushed aggressively by nursing schools at otherwise-reputable institutions.
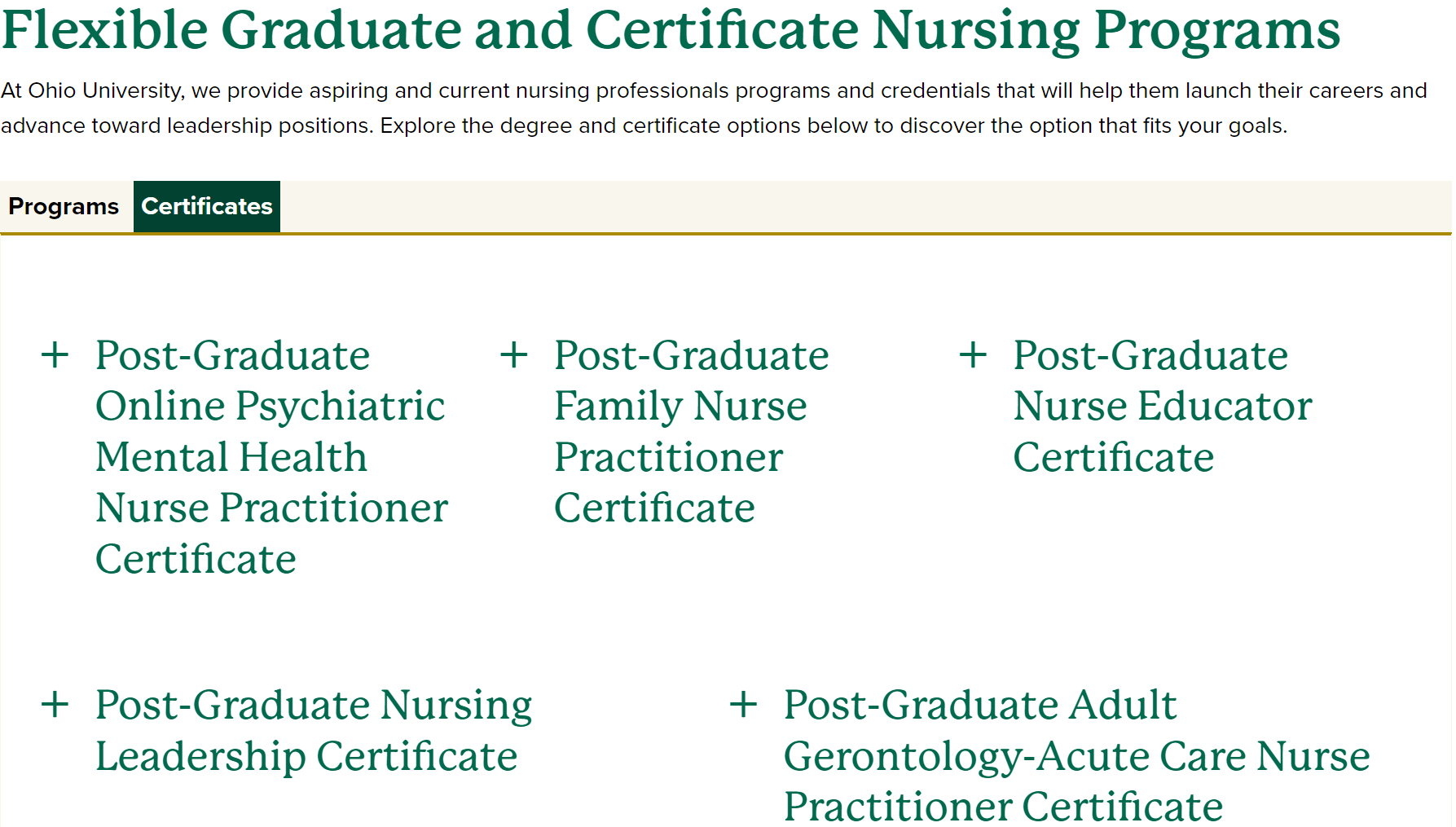
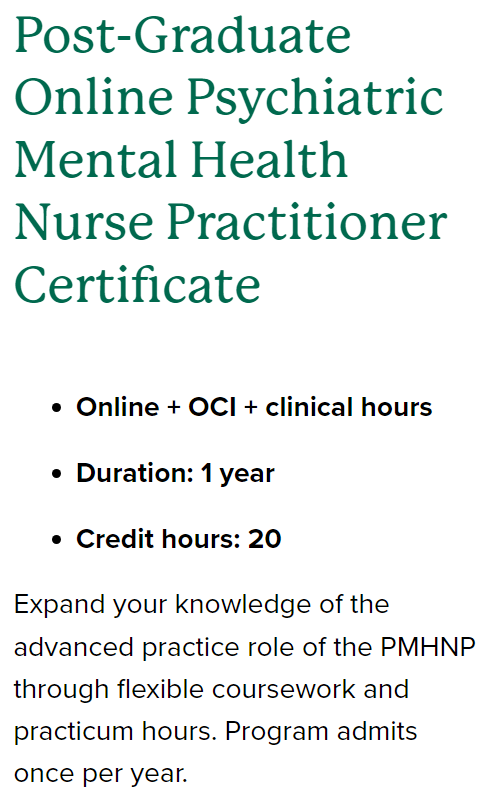
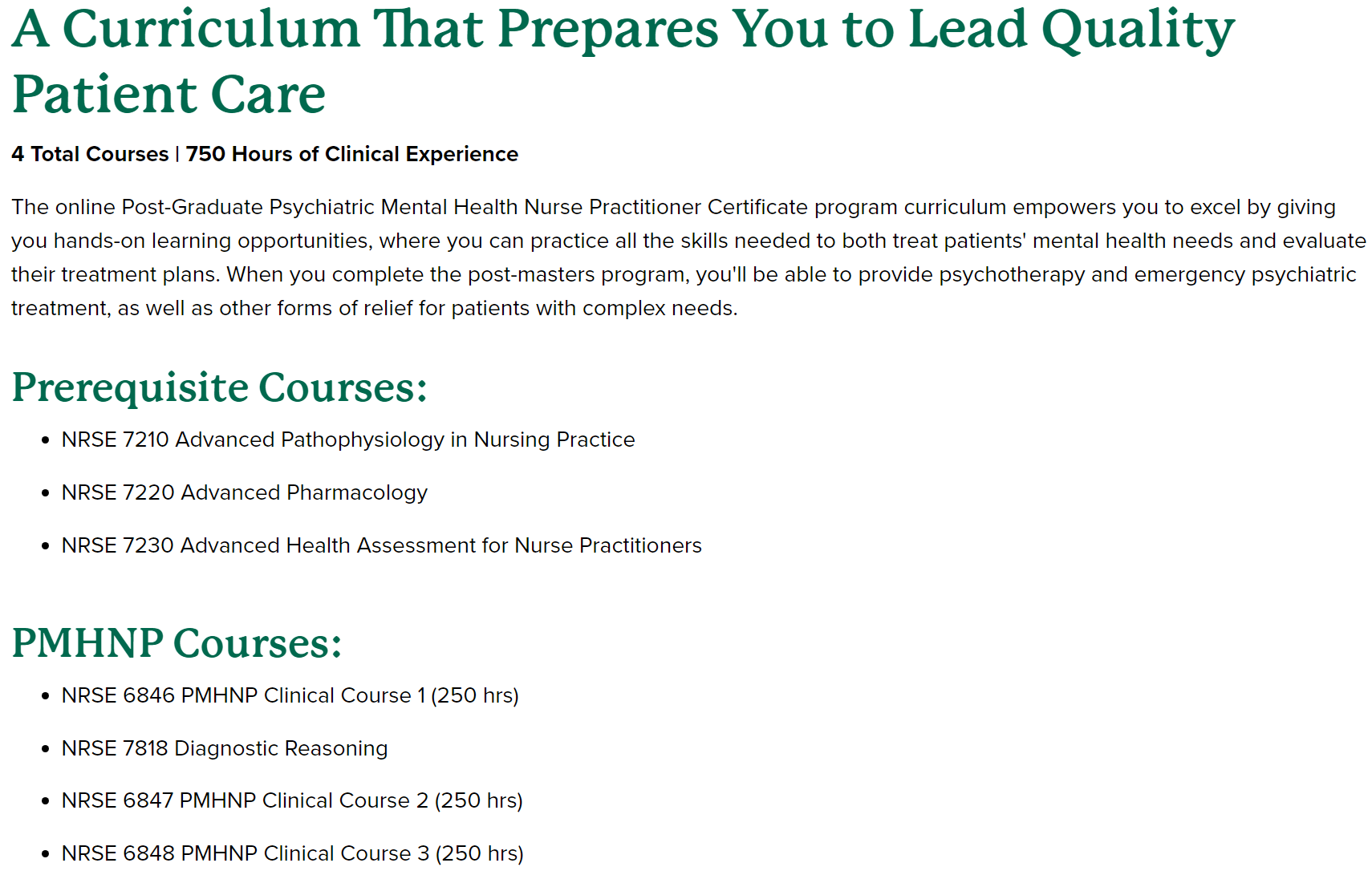
For example, Ohio University, which is also home to a reputable osteopathic medical school, offers a variety of online certificates in basically every fucking ice cream flavor imaginable (with the exception of women's health). For the low, low price of only $12,660, a year of your time, 20 credit hours in "Advanced Pathophysiology in Nursing Practice", "Advanced Pharmacology", "Advanced Health Assessment for Nurse Practitioners", only one PMHNP-specific course entitled "Diagnostic Reasoning", and an above-average 750 hours of "clinical experience", whatever the hell that is, Ohio University will happily sell you a certificate that allows you to re-invent yourself as a psychiatric-mental health nurse practitioner.
By contrast, physicians wishing to change specialties face the herculean prospect of having to apply, match into, and successfully complete a residency program in their newly chosen specialty, a process that requires a metric fuckton of planning. You can't just go and do some filler coursework for your online PMHNP certificate while still holding down a full-time job. For various reasons, including funding limitations, time and effort involved, and the fact that one would be competing with new medical school graduates for residency spots, only a minority of physicians choose to pursue a second residency, and the transition that often occurs is one from a more competitive specialty that requires a longer residency, such as general surgery, to a less-competitive specialty with shorter residency training such as family medicine.
And unlike the lax-to-nonexistent and poorly enforced "standards" for NP programs set by the Accreditation Commission for Education in Nursing (ACEN) and the Commission on Collegiate Nursing Education (CCNE), residency programs don't have much room to fuck around with the specific and stringent standards set by the Accreditation Council for Graduate Medical Education (ACGME), which is known to conduct unannounced site visits if it gets whiff of a residency program with compliance issues. How often is the ACEN/CCNE auditing the countless certificate programs offered by for-profit companies masquerading as educational institutions? How would you audit a 100% online program anyway?
Most significantly, the ACGME as well as the various constituent specialty boards under the American Board of Medical Specialties (ABMS) have highly specific rules and criteria for resident physicians switching to another training program as well as how much credit for patient encounters and procedures can be carried over to a new residency program from previously completed rotations. At most, one years' worth of credit might be given, meaning that a resident or attending physician training in a new program is looking at a minimum of two years and a few thousand more hours in full-time clinical training, not to mention the additional rigor of earning and maintaining an additional specialty board certification after completing a second residency. By contrast, the primary care NP you saw yesterday can decide to get a PMHNP certificate today like it's the new fucking ice cream flavor of the day.
So who would you rather see - a board-eligible/board-certified psychiatrist who devoted multiple years and thousands of hours in medical school and residency to hone their craft, or a fresh-meat nurse practitioner who got bored of their old job after a few months and decided to get a certificate and become a PMHNP on a whim? The answer to that question is pretty fucking obvious, isn't it?
