MidlevelWTF responds to AAPA's response to AAEM/RSA's Open Letter
💬 comments

Yesterday, the AAPA (technically AAPA President, Beth R. Smolko, DMSc, MMS, PA-C, DFAAPA) published a response to the recent AAEM/RSA Open Letter summarizing recent concerning trends in the field of emergency medicine, specifically the explosive growth of EM residency programs (particularly CMG-sponsored programs at for-profit hospitals) and the increasing number of patients in the emergency department seen by midlevel providers such as physician assistants and nurse practitioners. In case you didn't know what Beth Smolko and her AAPA co-conspirators think of physicians and how the AAPA has actively worked to exploit the COVID-19 pandemic to push for full practice authority, here's a quick overview:
With this in mind, let's take a closer look at the AAPA article. First off is the eyebrow-raising reference to the AAEM/RSA as a "student organization". We're going to stop you right fucking there, Beth. RSA = Resident and Student Association. For the record, there is an imperial shit-ton of residents who are members of AAEM/RSA, either individually or through residency program sponsorship. It really shouldn't need to be clarified, but residents are paid (arguably not enough) employees, and definitely not students. Leave it to a midlevel to entirely miss that distinction.

Smolko continues to take potshots, immediately claiming that it's "simply untrue" that "PAs and NPs have been “physician extenders” during physician shortages, but without a shortage, there is no longer a need for this “extension”. Well, Biggety Beth, may we suggest that you do some reading to refresh your memory on the history of your own profession? "The first educational program for physician assistants began in 1965 in response to a perceived shortage and maldistribution of physicians." Presumably to demonstrate the "importance" of PAs, she later mentions that "nearly 10% of the nation’s approximately 150,000 PAs practice in emergency medicine". Well, let's do some simple math here. Accepting this statistic as true, 10% of 150,000 is 15,000. If she had bothered actually reading ACEP's EM Physician: Workforce of the Future report (which is actually cited as a source by the AAPA), she would've seen the projection of almost 10,000 surplus EM-trained physicians within a decade. At that rate, it shouldn't take long take long to replace every single one of those all-important emergency PAs with an emergency P(hysician)!
The AAPA president also has the gall to label as "simply untrue" the statement that "graduating EM physicians are “significantly more qualified [than PAs and NPs] to fill these patient care roles.” Seriously, Beth? This is just a matter of common sense, unless you want to try refuting the axiom that people with more education, training, and experience are more qualified than people with less. We've already beat the MD/DO-versus-NP horse to death:
#EmergencyMedicine #ERDoc #BAFERD #NursePractitioner #NotEvenClose #NoComparison #PhysiciansLead #AskForAPhysician #StopScopeCreep #MedSchoolMatters #MedTwitter pic.twitter.com/ybE7tAHUvw
— Midlevel.WTF (@MidlevelWTF) April 13, 2021
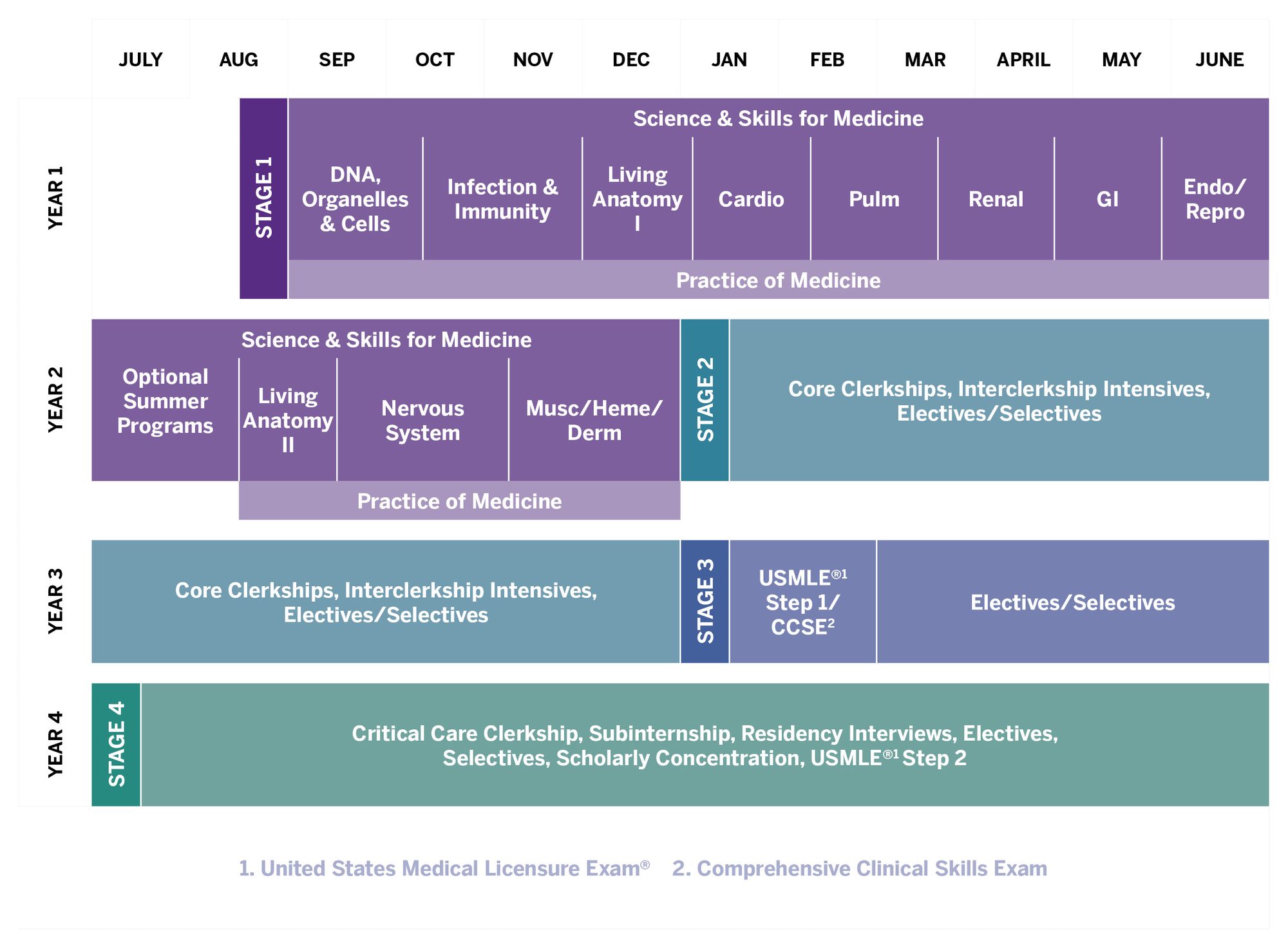
Now let's do a head-to-head comparison of physician versus physician assistant education. An attending emergency medicine physician must complete four years of medical school (typically divided into 2 preclinical science years followed by 2 years of core clerkships and specialty electives), followed by completion of 3- or 4-year residency in emergency medicine, possibly followed further by a subspecialty fellowship in a field like EMS, ultrasound, critical care, etc. This doesn't even begin to take into account the possibility of even more education through various dual-degree programs such as MD/PhD, MD/MBA, MD/MPH, MD/JD, etc.
After passing through a far less competitive admissions process, a typical physician assistant also undertakes a significantly more abbreviated curriculum. The first year is highly condensed and skimps significantly on basic sciences and pathophysiology, while the second year consists of core clerkships (usually in primary care specialties) supplemented by a small smattering of electives.
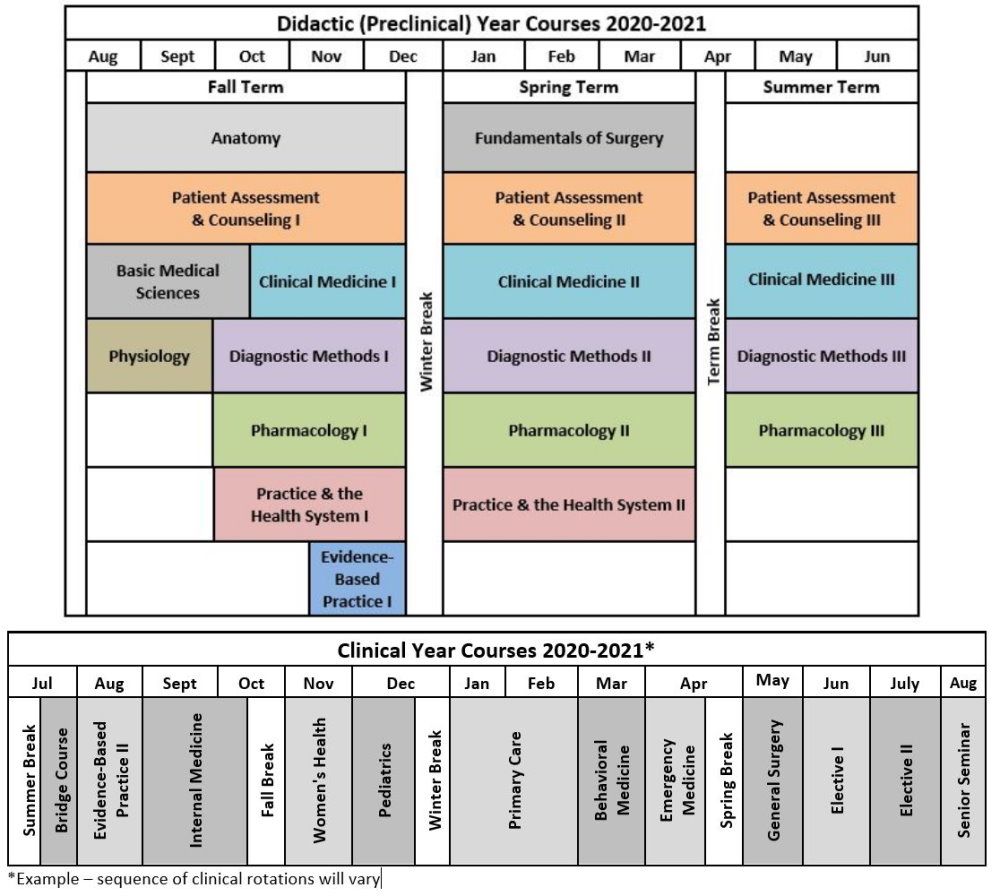
Most crucially, PAs are not required to complete further postgraduate training in the way that physicians are required to complete a categorical residency program in order to be board-eligible/board-certified in a specialty. Beth, can you really say with a straight face that a PA with possibly as little as two weeks' worth of emergency medicine clerkship under their belt is ready to start practicing in a real emergency department and start providing "high-quality patient care similar to that of physicians"? How about in an under-resourced rural ED environment with no specialty coverage that even a seasoned emergency physician would consider to be challenging? In emphasizing the importance of physician-led teams, the ACEP Workforce report explicitly states: "Physicians are trained to recognize the subtleties in patient presentations. They have more experience and training to appropriately triage patients to the correct provider." In no fucking way is a PA going to even be remotely as qualified as a newly-graduated emergency medicine physician. Give us a break with the fake news, Beth!
Make no mistake, the future of emergency medicine may be in dire straits if the corporatization and unchecked expansion of the specialty continues. But if the AAPA truly cared about high-quality patient care, they wouldn't be spending time writing propaganda hit pieces exaggerating their supposed irreplaceability and trying to draw false equivalences between physicians and physician assistants.
